Abstract
The increased IFN-g levels observed in acquired aplastic anemia (AA), have a crucial role in the immune destruction of the hematopoietic progenitors which subsequently lead to the clinical presentation of this rare and complicated disease. We and others have previously shown that the transcription factor T-bet is over-expressed in T cells from patients with AA. Recently it was shown that a subpopulation of B cells also express T-bet; these cells are characterized as age-associated B cells (ABCs) and express high levels of CD11c and CD19, and are negative for CD21. Stimulation of B cells leads to the formation of ABCs, which in turn "talk" to the T cells and stimulate them, leading to IFN-g production. IFN-g may lead to further induction of T-bet expressing B cells (ABCs). Ets-1 is an essential cofactor for STAT1 in the regulation of T-bet in ABCs. A small subset of CD4+helper T cells, circulating T follicular helper cells (Tfh) are also implicated in T-bet expression in ABCs. They are characterized by the surface expression of CXCR5, ICOS, and PD1, the transcription factor Bcl-6, and produce mainly IL-21, but also IL-17, IL-4, and IFN-γ. To date, there is no information on the expression of ABCs and Tfh cells in patients with aplastic anemia.
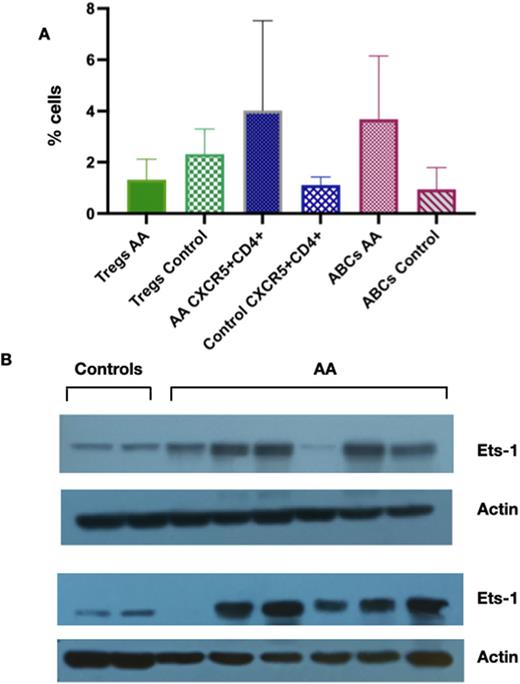
The current study population included 19 patients with AA and 20 healthy volunteers. The diagnosis of AA was based on the criteria of the International Agranulocytosis and Aplastic Anemia Study. Marrow cytogenetics were normal in all aplastic anemia cases and Fanconi anemia was excluded in all patients. Peripheral blood samples were obtained after written informed consent and using protocols approved by the institutional review board of the University of Patras Medical School, Greece. At the time of sampling, 17 out of 19 of the patients included in the study were at initial diagnosis before receiving any treatment and two patients were in complete remission and off any immunosuppressive treatment. The ABCs, Tfh, and regulatory T cell populations were examined using flow cytometry. We first measured the frequency of ABCs (results are in % ± SEM). All patients had significantly increased numbers of ABCs compared to healthy volunteers (3.68 ± 0.82% vs 0.94 ± 0.34%, p=0.022, Figure 1A). In the two cases in remission, the ABCs levels were lower than the levels of patients at diagnosis. We further examined if there were any differences in the percentages of T follicular helper cells; Patients also showed increased levels of Tfh cells compared to healthy controls (4.02± 1.01% vs 1.11 ± 0.10%, p=0.023, Figure 1A).
The patients showing increased levels of ABCs and Tfh cells were also examined for the presence of regulatory T cells (Tregs) as determined by the expression of CD4+ CD25hi , CD127low expression. As expected patients with aplastic anemia showed decreased levels of Tregs compared to healthy volunteers (1.31 ± 0.26 % vs 2.33 ± 0.36%, p=0.03, Figure 1A) .
To further explore the mechanism involved in the increased expression of these two cell populations in AA patients, we examined the intracellular Ets-1 protein levels. AA patients showed statistically significant increased Ets-1 protein levels compared to controls (western blot, Figure 1B). Ets-1 protein levels correlated with the increased ABCs counts. Stat-1 protein levels were comparable between patients and controls, as previously described.
In this study we explored the role of ABCs, the T-bet expressing B cells, in the immune pathogenesis of AA. We show for the first time that ABCs are increased along with increased pTfh cells, which are required for ABCs formation. The transcription factor Ets-1 is increased in AA patients and this could be one of the potential mechanisms for the increased ABCs. Whether these alterations are a consequence of increased IFN-g from polarized Th1 cells is not fully understood. One possible explanation could be that the IFN-g produced by activated T cells leads to increased numbers of circulating ABCs; these ABCs induce further the IFN-g production leading to a vicious cycle of IFN-g production in effect jeopardizing hematopoietic stem cell survival, leading to the clinical presentation of AA. Based on our results, it is proposed that T-bet has a central role not only in T but also in a small B cell subpopulation that seems central in AA pathogenesis. The development of agents that specifically target T-bet+ cells could possibly be used as novel therapeutic agents for AA but also for other autoimmune diseases.
Disclosures
Kattamis:BMS/Celgene: Consultancy, Honoraria, Research Funding; VERTEX: Consultancy, Honoraria; Chiesi: Honoraria; Novartis: Consultancy, Honoraria, Research Funding; ViFOR: Consultancy; IONIS: Consultancy; AGIOS Pharmaceuticals: Consultancy; AMGEN: Consultancy. Symeonidis:Astellas: Research Funding; WinMedica: Research Funding; Vianex: Research Funding; Servier SOBI: Membership on an entity's Board of Directors or advisory committees; Roche: Research Funding; Rafarm: Honoraria; Demo/Apopharma: Research Funding; Abbvie, Amgen, Astra-Zeneca, BMS, GenesisPharma, Gilead, Glaxo, Integris, Janssen, Novartis, Pfizer, Sanofi, Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. Diamantopoulos:Novartis, Roche, Janssen, BMS: Honoraria. Giannakoulas:JANSSEN: Honoraria, Other: travel expenses, Speakers Bureau; TAKEDA: Consultancy, Honoraria; AMGEN: Honoraria, Other: travel expenses; Integris: Consultancy, Honoraria; Genesis Pharma: Honoraria, Speakers Bureau. Viniou:ABBVIE, NOVARTIS, BMS,ASTRAZENECA, ASTELLAS GENESISPHARMA,: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal